As a gastroenterologist, I spend countless hours with patients who are frustrated, confused, and sometimes desperate to understand why their digestive system seems to be working against them. After decades of practice, one thing has become crystal clear: food is medicine, but it can also be poison. The difference often lies not just in what we eat, but in how our individual bodies respond to different foods.
Today, I want to cut through the noise of conflicting nutritional advice and give you my honest, evidence-based perspective on which foods genuinely support digestive health and which ones consistently cause problems for my patients.
The Foods That Heal: Your Digestive System’s Best Friends
Fermented Foods: Nature’s Probiotics
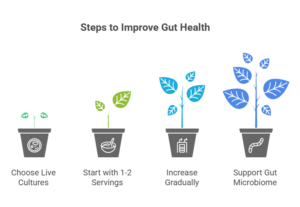
Let’s start with the superstars of digestive health: fermented foods. I’ve seen patients transform their gut health by simply incorporating these into their daily routine. Yogurt with live cultures, kefir, sauerkraut, kimchi, and miso aren’t just trendy—they’re scientifically proven to support your gut microbiome.
The key is choosing fermented foods with live, active cultures. That jar of sauerkraut sitting on the shelf at room temperature? It’s been pasteurized, killing the beneficial bacteria. Look for refrigerated versions that explicitly state “live cultures” on the label.
Key Points:
- Choose refrigerated fermented foods with “live cultures” on the label
- Pasteurized versions lack beneficial bacteria
- Start with 1-2 servings daily and increase gradually
I often tell patients to think of fermented foods as sending reinforcements to their gut army. These beneficial bacteria help crowd out harmful microorganisms, support immune function, and even produce vitamins like B12 and K2.
Fiber: The Unsung Hero
Despite what diet culture might tell you, fiber isn’t just about staying regular (though that’s important too). Soluble fiber, found in oats, beans, apples, and psyllium husk, acts like a sponge in your digestive tract, slowing down digestion and helping stabilize blood sugar levels.
Insoluble fiber from vegetables, whole grains, and nuts adds bulk to stool and helps food move through your system efficiently. But here’s what many people don’t realize: fiber is also food for your beneficial gut bacteria. When these bacteria ferment fiber, they produce short-chain fatty acids that reduce inflammation and support colon health.
Remember:
- Soluble fiber = found in oats, beans, apples (slows digestion)
- Insoluble fiber = found in vegetables, whole grains (adds bulk)
- Both types feed beneficial gut bacteria
- Increase gradually to avoid bloating
The caveat? Increase fiber gradually. I’ve seen too many well-intentioned patients go from zero to hero overnight, only to end up bloated and gassy. Start with small amounts and let your digestive system adapt.
Omega-3 Rich Foods: The Anti-Inflammatory Powerhouses
Chronic inflammation is at the root of many digestive disorders, from inflammatory bowel disease to irritable bowel syndrome. Fatty fish like salmon, mackerel, and sardines provide omega-3 fatty acids that help reduce this inflammation.
Best Sources:
- Fatty fish: salmon, mackerel, sardines (twice weekly)
- Plant-based: walnuts, flaxseeds, chia seeds
- Consider high-quality fish oil if you don’t eat fish
If you’re not a fish eater, walnuts, flaxseeds, and chia seeds offer plant-based omega-3s, though they’re not quite as readily absorbed as their fish-based counterparts. I often recommend patients aim for fatty fish twice a week or consider a high-quality fish oil supplement.
Bone Broth and Collagen-Rich Foods
While the research is still evolving, I’ve observed that patients who regularly consume bone broth or collagen-rich foods often report improvements in their digestive symptoms. These foods may help support the gut lining, which acts as a barrier between your digestive tract and the rest of your body.
The amino acids in collagen, particularly glycine and glutamine, appear to support gut barrier function. While more research is needed, the anecdotal evidence from my practice is compelling enough that I often suggest patients give it a try.
The Foods That Harm: The Usual (and Unusual) Suspects
Ultra-Processed Foods: The Silent Destroyers
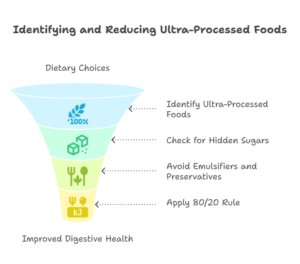
If I could eliminate one category of food from my patients’ diets, it would be ultra-processed foods. These aren’t just obviously unhealthy options like chips and cookies—they include many foods marketed as healthy, like flavored yogurts loaded with sugar, processed meats, and even some plant-based meat alternatives.
Ultra-processed foods often contain emulsifiers, preservatives, and artificial additives that can disrupt the gut microbiome and increase intestinal permeability. They’re also typically high in sugar and low in fiber, creating the perfect storm for digestive dysfunction.
Watch Out For:
- Foods with long ingredient lists you can’t pronounce
- Emulsifiers and preservatives that disrupt gut bacteria
- “Healthy” processed foods with hidden sugars
- Apply the 80/20 rule: 80% whole foods, 20% flexibility
The 80/20 rule works well here: aim for 80% whole, minimally processed foods, and don’t stress about the remaining 20%.
Sugar and Artificial Sweeteners: The Double-Edged Sword
Excessive sugar feeds harmful bacteria and yeast in the gut, potentially leading to overgrowth and inflammation. But artificial sweeteners aren’t necessarily the answer. Studies suggest that some artificial sweeteners can negatively alter gut bacteria composition.
Sugar alcohols like sorbitol and xylitol, found in sugar-free gum and candies, can cause digestive upset in many people, particularly those with sensitive stomachs or IBS.
The Reality:
- Sugar feeds harmful gut bacteria and yeast
- Artificial sweeteners can disrupt gut microbiome
- Sugar alcohols (sorbitol, xylitol) cause digestive upset in many
- Reduce overall sweetness gradually instead of substituting
My advice? Reduce overall sweetness gradually, allowing your taste buds to adapt. When you do use sweeteners, stick to small amounts of natural options like honey or maple syrup.
Gluten: Not Just a Problem for Celiacs
While only about 1% of the population has celiac disease, I see many more patients who experience digestive improvements when they reduce or eliminate gluten. Non-celiac gluten sensitivity is real, though we don’t fully understand the mechanisms behind it.
That said, many “gluten-free” processed foods are nutritionally inferior to their gluten-containing counterparts and often higher in sugar and additives. If you’re going gluten-free, focus on naturally gluten-free whole foods rather than processed alternatives.
High-FODMAP Foods: The Hidden Triggers
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are certain types of carbohydrates that can trigger symptoms in people with IBS and other functional digestive disorders. These include certain fruits (like apples and pears), vegetables (like onions and garlic), legumes, and dairy products.
Here’s the important part: FODMAPs aren’t inherently bad. They’re actually beneficial for most people. But if you have IBS, they can ferment in your gut and cause bloating, gas, and changes in bowel habits.
Important Facts:
- FODMAPs aren’t bad for everyone—only IBS sufferers typically
- Common triggers: apples, pears, onions, garlic, beans, dairy
- Low-FODMAP diet should be professionally guided
- Goal is to identify personal triggers, then gradually reintroduce
A low-FODMAP diet should be done under professional guidance and isn’t meant to be followed long-term. The goal is to identify your specific triggers, then gradually reintroduce foods to determine your personal tolerance levels.
The Individual Factor: Why One Size Doesn’t Fit All
This is perhaps the most important point I can make: there’s no single “perfect” diet for everyone. I’ve seen patients thrive on diets that would make others miserable. Your genetics, gut microbiome, stress levels, medical history, and even your cultural background all influence how you respond to different foods.
What works for your neighbor, your favorite influencer, or even your doctor might not work for you. This is why I encourage patients to become their own food detectives. Keep a food and symptom diary for a few weeks. Look for patterns. Pay attention to how different foods make you feel, not just immediately after eating, but over the following 24-48 hours.
Beyond Individual Foods: The Bigger Picture
While focusing on specific foods is important, I want to emphasize that how you eat matters as much as what you eat. Eating slowly, chewing thoroughly, managing stress, staying hydrated, and maintaining regular meal times all support digestive health.
The Mediterranean diet consistently comes out on top in research studies, not because of any single superfood, but because it emphasizes whole foods, healthy fats, moderate portions, and the social aspect of sharing meals.
Practical Steps to Get Started
Start small. Choose one healing food to add to your diet this week and one harmful food to reduce or eliminate. Maybe that’s adding a small serving of fermented vegetables to your lunch and swapping out your afternoon processed snack for a handful of nuts.
Listen to your body. If a food consistently makes you feel unwell, regardless of how healthy it’s supposed to be, trust your experience.
Action Plan:
- Add one healing food this week
- Remove or reduce one harmful food
- Keep a food and symptom diary for 2-3 weeks
- Give changes 4-6 weeks to show effects
- Listen to your body over popular advice
Be patient. Digestive healing takes time. Your gut microbiome didn’t change overnight, and it won’t heal overnight either. Give dietary changes at least 4-6 weeks to show their effects.
Take Control of Your Digestive Health
If you’re reading this and struggling with persistent digestive symptoms, don’t let another month pass wondering if what you’re experiencing is “normal.” Bloating after every meal isn’t normal. Chronic stomach pain isn’t something you have to live with. Irregular bowel habits that interfere with your daily life deserve attention.
Many digestive issues are highly treatable when properly diagnosed and managed. The right dietary approach, combined with professional guidance, can transform not just your digestive health but your overall quality of life.
The discomfort of unaddressed digestive problems affects your energy, mood, social life, and productivity. The relief that comes from understanding your body and eating in a way that supports your unique digestive system is life-changing.
Dr. Preetha is committed to helping patients achieve optimal digestive health through personalized care and evidence-based treatment. If you’re experiencing ongoing digestive symptoms or want to optimize your gut health, contact our office to schedule your consultation.