If you feel like you’re constantly battling stomach discomfort—bloating after meals, cramping, nausea, or unpredictable bathroom trips—you’re not alone. One of the most common complaints I hear as a gastroenterologist is: “Doctor, it seems like everything I eat upsets my stomach.”
This frustrating experience can make mealtimes stressful and leave you wondering if you’ll ever enjoy food again without consequences. The good news is that persistent digestive upset usually has identifiable causes, and once you understand what’s triggering your symptoms, you can take steps to feel better.
Let’s explore the most common culprits behind chronic stomach upset and how to identify which one might be affecting you.
Understanding Your Digestive Symptoms
Before we dive into specific causes, it’s important to recognize that “upset stomach” can mean different things to different people. Common symptoms include:
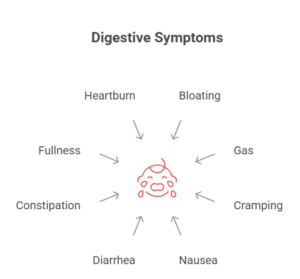
- Bloating and abdominal distension
- Gas and flatulence
- Cramping or abdominal pain
- Nausea
- Diarrhea or loose stools
- Constipation
- Feeling uncomfortably full after eating
- Heartburn or acid reflux
The timing, location, and type of symptoms you experience can provide valuable clues about what’s causing your digestive distress.
Common Culprit #1: Food Intolerances
Food intolerances are one of the most frequent causes of chronic digestive upset, and they’re often confused with food allergies, though they’re quite different.
Lactose Intolerance
Lactose intolerance affects approximately 65% of the global population and occurs when your body doesn’t produce enough lactase, the enzyme needed to digest lactose (milk sugar). Symptoms typically appear 30 minutes to 2 hours after consuming dairy products and include bloating, gas, cramping, and diarrhea.
Interestingly, many people develop lactose intolerance later in life, even if they tolerated dairy perfectly well as children. This happens because lactase production naturally decreases with age.
Fructose Malabsorption
Fructose is a sugar found naturally in fruits, honey, and many processed foods (as high-fructose corn syrup). Some people have difficulty absorbing fructose in the small intestine, leading to bloating, gas, and diarrhea. This condition is more common than many realize and can make healthy foods like apples, pears, and watermelon problematic.
Other Common Intolerances
- Gluten sensitivity (non-celiac): Causes digestive symptoms similar to celiac disease but without intestinal damage
- Histamine intolerance: Results from difficulty breaking down histamine in certain foods
- FODMAPs: Short-chain carbohydrates that are poorly absorbed and can trigger IBS symptoms
Common Culprit #2: Functional Digestive Disorders
Sometimes, digestive upset occurs not because of what you’re eating, but because of how your digestive system is functioning.
Irritable Bowel Syndrome (IBS)
IBS affects 10-15% of adults and is characterized by chronic abdominal pain, bloating, and changes in bowel habits without any visible damage to the digestive tract. The exact cause isn’t fully understood, but IBS involves abnormal gut-brain communication, visceral hypersensitivity (increased pain sensation), and altered gut motility.
People with IBS often report that many different foods trigger symptoms, making it feel like “everything” bothers them. This happens because IBS involves a heightened sensitivity of the digestive system rather than specific food reactions.
Functional Dyspepsia
This condition causes persistent upper abdominal discomfort, early satiety (feeling full quickly), and bloating without an identifiable cause. It affects about 20% of people worldwide and can make eating feel like a chore rather than a pleasure.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO occurs when excessive bacteria grow in the small intestine, where bacteria levels should normally be low. These bacteria ferment food, producing gas and leading to bloating, pain, and diarrhea. SIBO can cause symptoms after eating almost any food, particularly carbohydrates.
Common Culprit #3: Eating Habits and Lifestyle Factors
Sometimes the problem isn’t what you eat but how you eat.
Eating Too Quickly
When you eat rapidly, you swallow more air, which contributes to bloating and gas. You also don’t chew food thoroughly, forcing your digestive system to work harder. Additionally, eating quickly often leads to overeating because your brain doesn’t have time to register fullness signals.
Eating Large Meals
Your stomach can only comfortably hold a certain amount of food. Overfilling it causes distension, discomfort, and can trigger reflux. Large, heavy meals also slow digestion, leading to prolonged feelings of fullness and bloating.
Eating Late at Night
Late-night eating doesn’t give your body adequate time to digest before lying down. This can worsen reflux symptoms and disrupt sleep quality, which in turn affects digestive health.
Chronic Stress and Anxiety
The gut-brain connection is powerful. Chronic stress affects gut motility, increases inflammation, and can trigger or worsen conditions like IBS. Many people notice their digestive symptoms flare during stressful periods, regardless of what they eat.
Common Culprit #4: Underlying Medical Conditions
Persistent digestive upset can signal underlying medical conditions that require diagnosis and treatment.
Gastroesophageal Reflux Disease (GERD)
GERD occurs when stomach acid frequently flows back into the esophagus, causing heartburn, nausea, and discomfort after eating. Many foods can trigger or worsen GERD symptoms, including fatty foods, spicy foods, caffeine, alcohol, and acidic foods.
Celiac Disease
Unlike gluten sensitivity, celiac disease is an autoimmune condition where gluten triggers immune system damage to the small intestine. It affects about 1% of the population and requires strict, lifelong gluten avoidance. Symptoms include diarrhea, bloating, fatigue, and nutrient deficiencies.
Inflammatory Bowel Disease (IBD)
Conditions like Crohn’s disease and ulcerative colitis cause chronic inflammation in the digestive tract. While these conditions involve more than just food reactions, certain foods can trigger symptom flares. IBD requires specialized medical treatment.
Gastroparesis
This condition involves delayed stomach emptying, causing nausea, vomiting, bloating, and early satiety. People with gastroparesis often feel like every meal sits heavily in their stomach for hours.
H. pylori Infection
Helicobacter pylori is a bacteria that infects the stomach lining and can cause chronic indigestion, nausea, and abdominal pain. It’s a common cause of peptic ulcers and can make you feel sick after eating.
Common Culprit #5: Medications
Many common medications can cause digestive side effects that make it seem like food is the problem when actually, it’s the medication.
Common Offenders Include:
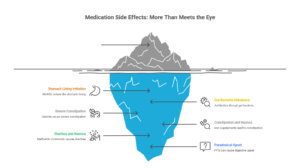
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Can irritate the stomach lining
- Antibiotics: Disrupt gut bacteria balance
- Opioids: Cause severe constipation
- Iron supplements: Lead to constipation and nausea
- Metformin: Commonly causes diarrhea and nausea
- Proton pump inhibitors (PPIs): Can paradoxically cause digestive upset in some people
If you started experiencing digestive symptoms after beginning a new medication, discuss alternatives with your doctor.
Common Culprit #6: Insufficient Digestive Enzymes
As we age, our bodies may produce fewer digestive enzymes needed to break down food efficiently. This can lead to feelings of indigestion, bloating, and discomfort after eating, particularly after fatty or protein-rich meals.
Conditions like chronic pancreatitis, cystic fibrosis, or pancreatic insufficiency can also affect enzyme production, making proper digestion difficult.
How to Identify Your Specific Triggers
If everything seems to upset your stomach, systematic investigation is key to finding answers.
Keep a Detailed Food and Symptom Diary
Track what you eat, when you eat, portion sizes, and when symptoms occur. Also note stress levels, sleep quality, and medications. Patterns often emerge after a few weeks that can help identify triggers.
Try an Elimination Diet (Under Medical Supervision)
Elimination diets involve removing common trigger foods for several weeks, then systematically reintroducing them to identify which ones cause symptoms. This should be done with guidance from a healthcare provider or dietitian to ensure nutritional adequacy.
Consider Timing and Context
Pay attention to whether symptoms relate to specific foods or to eating patterns. Do you feel worse after eating quickly? After large meals? During stressful periods? This information is valuable for diagnosis.
Get Proper Testing
Don’t guess about serious conditions. Testing options include:
- Lactose breath test: For lactose intolerance
- Celiac blood tests and endoscopy: For celiac disease
- Hydrogen breath test: For SIBO or fructose malabsorption
- Stool tests: For infections, inflammation, or malabsorption
- Upper endoscopy or colonoscopy: To visualize the digestive tract
- Gastric emptying study: For gastroparesis
Taking Action: Steps Toward Relief
Start With These Foundational Changes:
- Eat smaller, more frequent meals rather than large meals
- Slow down and chew thoroughly – aim for 20-30 minutes per meal
- Stay hydrated throughout the day, not just at meals
- Manage stress through meditation, exercise, or counseling
- Avoid eating within 3 hours of bedtime
- Keep a food diary to identify patterns
- Limit known irritants like alcohol, caffeine, and spicy foods while investigating
When to See a Gastroenterologist
Schedule an appointment if you experience:
- Persistent symptoms lasting more than a few weeks
- Unintended weight loss
- Blood in stool
- Severe abdominal pain
- Persistent vomiting
- Difficulty swallowing
- Symptoms that interfere with daily life
- Family history of digestive diseases
The Path to Comfortable Eating
Living with chronic digestive upset is frustrating and can significantly impact quality of life. The feeling that “everything” bothers your stomach is overwhelming, but with proper investigation and targeted treatment, most people can identify their triggers and find substantial relief.
Remember that everyone’s digestive system is unique. What bothers your friend might not bother you, and vice versa. This isn’t about following a one-size-fits-all approach—it’s about understanding your individual digestive health and working with healthcare providers to develop a personalized management plan.
The goal isn’t perfection; it’s progress. Even identifying and eliminating just a few major triggers can dramatically improve your symptoms and relationship with food.
Moving Forward With Hope
If you’re tired of feeling like you can’t eat anything without consequences, know that answers exist. Modern gastroenterology offers sophisticated diagnostic tools and effective treatments for virtually every digestive condition. The key is getting proper evaluation rather than suffering in silence or unnecessarily restricting your diet.
Your digestive system wants to work properly—sometimes it just needs help identifying and addressing what’s getting in the way.
Dr. Preetha is committed to helping patients achieve optimal digestive health through personalized care and evidence-based treatment. If you’re experiencing ongoing digestive symptoms or want to optimize your gut health, contact our office to schedule your consultation.
You deserve to enjoy food again without fear or discomfort. With the right approach and professional guidance, that goal is entirely achievable.