Something concerning is happening to our digestive systems, and most people don’t even realize it. As a gastroenterologist, I’m seeing more patients in their 20s and 30s with digestive problems that used to appear mainly in middle age or later. Young, otherwise healthy people are experiencing chronic bloating, irregular bowel movements, unexplained abdominal pain, and food sensitivities that seem to appear out of nowhere.
This isn’t coincidence. The way we live in 2026 has fundamentally changed from even just a decade ago, and our digestive systems are struggling to keep up. The habits we’ve normalized—behaviors we don’t even question anymore—are quietly wreaking havoc on our gut health. The scary part? Most of these damaging habits feel completely ordinary and harmless.
Let me walk you through what’s actually happening to your digestive system in modern life, and more importantly, what you can do about it before the damage becomes serious.
The Screen Time Epidemic That’s Destroying Your Digestion
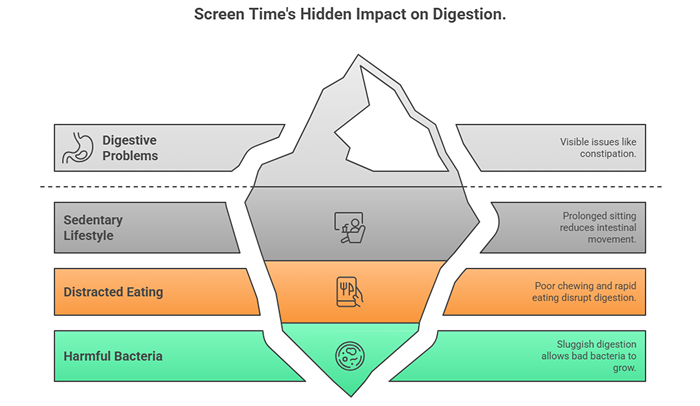
We’re spending more time on screens than ever before. Between work computers, smartphones, tablets, and streaming services, the average person now logs over 11 hours of screen time daily. And almost nobody connects this to their digestive problems.
Here’s what’s happening: when you’re glued to screens, you’re not moving. You’re sitting. For hours and hours, day after day. This sedentary lifestyle has direct consequences for your digestive system.
Your intestines rely on physical movement to function properly. When you walk, stretch, or engage in any physical activity, your body movement stimulates intestinal contractions that push food and waste through your system. This is called peristalsis. When you sit motionless for extended periods, this natural movement slows dramatically.
The result? Constipation becomes your new normal. Food moves through your system sluggishly, spending far too long in your intestines. This extended transit time allows harmful bacteria to flourish and creates the perfect environment for digestive issues.
But it gets worse. Most screen time happens while eating. You scroll through your phone during breakfast. You watch videos during lunch. You binge shows during dinner. This distracted eating means you’re not chewing properly, you’re eating too quickly, and you’re completely disconnected from your body’s hunger and fullness signals.
When you don’t chew food thoroughly, your stomach and intestines must work much harder to break it down. Large food particles can irritate the digestive lining and feed the wrong types of gut bacteria. The combination of poor chewing and rapid eating also causes you to swallow excessive air, leading to bloating and that uncomfortable sensation of constant stomach rumbling many people now experience.
Ultra-Processed Foods Have Become Our Default
Walk into any home in 2026 and open the pantry. What do you find? Boxes, bags, and packages of ultra-processed foods designed for convenience. These products now make up nearly 60% of the average person’s daily caloric intake.
Ultra-processed foods aren’t just “processed”—they’re products that have been stripped of nutrients, loaded with additives, and engineered to be hyperpalatable and shelf-stable. Think packaged snacks, frozen meals, breakfast cereals, processed meats, sugary drinks, and most restaurant food.
Your gut bacteria are starving. Literally. Beneficial gut bacteria need fiber from whole plant foods to survive. When you consume mostly ultra-processed foods with minimal fiber, these good bacteria die off. Meanwhile, bacteria that thrive on sugar and simple carbohydrates multiply rapidly.
This imbalance—called dysbiosis—has cascading effects throughout your digestive system and entire body. It contributes to inflammation, weakens your intestinal barrier, impairs nutrient absorption, and even affects your mood and mental health through the gut-brain connection.
The additives in these foods compound the problem. Emulsifiers, commonly used to create smooth textures, can actually damage the mucus layer protecting your intestinal lining. Artificial sweeteners alter your gut bacteria composition. Preservatives that keep food “fresh” for months also kill beneficial bacteria in your digestive tract.
Many people unknowingly develop conditions like bile acid malabsorption partly due to the chronic digestive stress created by these processed foods. When your gut is constantly inflamed and imbalanced, various absorption and digestive processes start breaking down.
The Stress Pandemic Nobody’s Addressing
If I had to identify one factor destroying gut health more than any other in 2026, it would be chronic, unrelenting stress. We’re more stressed than humans have ever been, and we’re wearing this stress like a badge of honor rather than recognizing it as the health crisis it is.
Your digestive system and brain are intimately connected through what scientists call the gut-brain axis. When you’re stressed, your body diverts resources away from digestion to prepare for “fight or flight.” This was useful when stress meant facing an immediate physical threat. But in 2026, stress is constant—work deadlines, financial pressure, social media comparison, political anxiety, environmental concerns.
Chronic stress fundamentally alters how your digestive system functions. It slows stomach emptying. It changes the composition of your gut bacteria. It increases intestinal permeability, allowing partially digested food particles and bacteria to leak into your bloodstream and trigger inflammation.
Many digestive conditions that used to be relatively rare are now epidemic, and stress is a major contributor. People are developing symptoms of ulcers and other stress-related digestive problems at younger and younger ages.
The stress response also affects your eating habits. Stress eating is real—when cortisol floods your system, you crave high-calorie, high-sugar foods. These stress-induced food choices further damage your gut health, creating a vicious cycle.
Sleep Deprivation Is Wrecking Your Gut
In our always-on, productivity-obsessed culture, sleep has become optional. The average person in 2026 sleeps just under 6 hours nightly—far below the 7-9 hours our bodies need.
Your gut bacteria operate on circadian rhythms just like you do. Different bacterial species become active at different times of day. When you consistently sleep too little or at irregular times, you disrupt these natural cycles.
Research shows that even a few nights of poor sleep can alter your gut microbiome composition. Chronic sleep deprivation causes long-term changes that promote inflammation, impair nutrient absorption, and increase your risk of digestive disorders.
Sleep deprivation also affects the hormones that regulate appetite and metabolism. When you’re sleep-deprived, you produce more ghrelin (the hunger hormone) and less leptin (the fullness hormone). This drives you to eat more, particularly high-calorie foods, compounding the damage to your digestive system.
The Antibiotic Overuse Crisis
Antibiotics save lives—there’s no question about that. But we’ve been using them far too casually for far too long, and our gut health is paying the price.
Every course of antibiotics is like dropping a bomb on your gut microbiome. Antibiotics don’t distinguish between harmful bacteria causing your infection and beneficial bacteria supporting your digestion. They kill everything. While your gut can recover, repeated antibiotic use—which many people experience throughout childhood and adulthood—creates lasting changes.
Children who receive multiple courses of antibiotics early in life show altered gut bacteria composition that persists into adulthood. These early disruptions are linked to increased rates of allergies, inflammatory bowel disease, and metabolic problems later in life.
Beyond direct antibiotic use, we’re also exposed through our food supply. Livestock raised for meat are routinely given antibiotics, and residues end up in the meat we consume. This low-level chronic exposure contributes to microbiome disruption.
The Dehydration Default
Despite water bottles being everywhere in 2026, chronic dehydration is incredibly common. Many people subsist primarily on coffee, energy drinks, and other caffeinated or sugary beverages, barely drinking plain water at all.
Your digestive system needs adequate water to function. Water helps produce the mucus that protects your stomach lining. It’s necessary for digestive enzymes to work properly. It keeps stool soft enough to pass comfortably.
When you’re chronically dehydrated, constipation becomes inevitable. Your colon extracts every bit of water it can from waste, creating hard, difficult-to-pass stools. This straining can lead to hemorrhoids and, over time, may contribute to developing hiatal hernia symptoms as increased abdominal pressure affects the area where your esophagus meets your stomach.
The beverages people choose instead of water often make things worse. Caffeinated drinks are diuretics that actually increase fluid loss. Sugary drinks feed harmful bacteria and contribute to inflammation. Alcohol irritates the digestive lining and impairs nutrient absorption.
The Meal Timing Mess
Our ancestors ate at relatively consistent times, aligned with daylight hours. In 2026, meal timing has become chaotic. People skip breakfast, grab lunch at their desk at random times, snack constantly, and eat dinner at 10 PM while binge-watching shows.
Your digestive system operates on predictable rhythms. Digestive enzymes and hormones are produced in anticipation of meals at regular times. When eating times are erratic, this preparation doesn’t happen properly.
Late-night eating is particularly problematic. Eating within three hours of bedtime means you’re trying to sleep while your digestive system is actively working. This contributes to acid reflux, disrupts sleep quality, and may promote weight gain since your metabolism slows at night.
Constant snacking—which food companies actively encourage—means your digestive system never gets a break. You’re always in “fed state,” which doesn’t allow for the natural cleansing waves that sweep through your digestive tract between meals, clearing out debris and bacteria.
The Exercise Deficit
The World Health Organization recommends at least 150 minutes of moderate exercise weekly. Most people in 2026 get maybe a quarter of that. We’ve engineered physical activity almost completely out of daily life.
Exercise isn’t just good for your cardiovascular system and muscles—it’s crucial for digestive health. Physical activity stimulates intestinal contractions, helping food move through your system efficiently. It reduces stress and its harmful effects on digestion. It promotes healthy gut bacteria diversity.
People who exercise regularly have significantly lower rates of constipation, inflammatory bowel conditions, and colon cancer compared to sedentary individuals. The digestive benefits of exercise are profound and well-documented, yet most people never connect their lack of movement to their digestive complaints.
The Supplement Trap
Walk through any health store or scroll through social media in 2026, and you’ll be bombarded with supplement advertisements promising to fix your gut. Many people now take handfuls of supplements daily, often without medical guidance.
Here’s the uncomfortable truth: most supplements aren’t regulated the way medications are. What’s on the label may not match what’s in the bottle. Some supplements contain contaminants or additives that actually harm your gut. Others interact with medications or create imbalances.
The supplement industry has convinced people that pills can compensate for poor diet and lifestyle habits. They can’t. No probiotic supplement can overcome the damage done by chronic stress, poor sleep, ultra-processed foods, and sedentary living.
That’s not to say all supplements are useless—some people benefit from specific supplementation under medical supervision. But the idea that everyone needs to take multiple gut health supplements is marketing, not medicine.
What You Can Actually Do About It
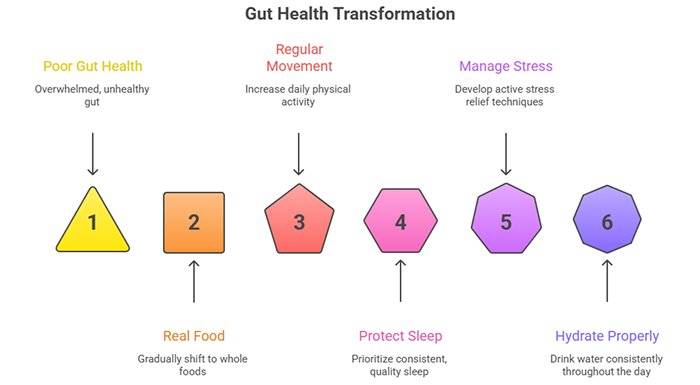
I know this all sounds overwhelming. The modern world seems designed to destroy your gut health. But you’re not powerless. Small, consistent changes make significant differences.
Start with real food. You don’t need to become a perfect clean eater overnight. Just gradually shift your diet toward more whole, unprocessed foods. Add vegetables to meals you’re already eating. Choose fruit instead of packaged snacks. Cook at home more often. Each small change helps.
Move your body regularly. You don’t need to become a gym fanatic. A 30-minute walk daily provides substantial digestive benefits. Take the stairs. Park farther away. Stand while working. Any increase in movement helps.
Protect your sleep. Make sleep a genuine priority. Create a consistent bedtime routine. Keep your bedroom cool and dark. Put screens away an hour before bed. Your gut will thank you.
Manage stress actively. Stress won’t disappear, but you can develop better ways to handle it. Try meditation, deep breathing, or therapy. Find stress relief that works for you and practice it consistently.
Hydrate properly. Carry a water bottle. Set reminders to drink if necessary. Notice when you’re thirsty and actually drink water instead of reaching for coffee or soda.
Establish meal routines. Try to eat at roughly the same times daily. Stop eating at least three hours before bed. Minimize snacking between meals.
Be skeptical of quick fixes. Be wary of products and programs promising miraculous gut healing. Real improvement comes from sustained lifestyle changes, not expensive supplements or restrictive diets.
When to Seek Professional Help
These lifestyle changes help prevent damage and support healing, but sometimes professional evaluation is necessary. See a gastroenterologist if you experience:
- Persistent digestive symptoms lasting more than a few weeks
- Blood in your stool
- Unintentional weight loss
- Severe pain
- Symptoms that significantly impact your daily life
Don’t wait until problems become severe. Early intervention prevents complications and improves outcomes.
The Bottom Line
Your gut health is probably worse in 2026 than it would have been if you’d lived in a different era. That’s not your fault—modern life creates perfect conditions for digestive problems. But recognizing the specific habits damaging your digestion empowers you to make different choices.
You can’t completely opt out of modern life, but you can be more mindful about protecting your digestive health within it. Small changes compound over time. Start somewhere. Your gut—and your overall health—will thank you for years to come.
The future of your digestive health isn’t predetermined. The choices you make today shape how your gut functions tomorrow. Choose wisely.
Expert Digestive Health Support
If you’re experiencing persistent digestive problems or want personalized guidance for optimizing your gut health, Dr. Preetha Thomas, specialist gastroenterologist in Pretoria, provides comprehensive evaluation and evidence-based treatment plans tailored to modern lifestyle challenges.
Contact us today to schedule your consultation.