I want to talk to you about something that’s become incredibly common but often goes unnoticed until it’s discovered by accident—fatty liver disease. If you’re reading this, chances are you’ve either been diagnosed with it yourself, or someone you know has. And honestly, that’s not surprising anymore.
Recent studies show that fatty liver now affects one out of every three people. Yes, you read that right. One in three. This number is even higher in certain populations, with research indicating a particularly sharp rise among Indian communities. When a condition becomes this widespread, we can no longer dismiss it as rare or unusual. It’s become a public health concern that deserves our attention.
What Exactly Is Fatty Liver?
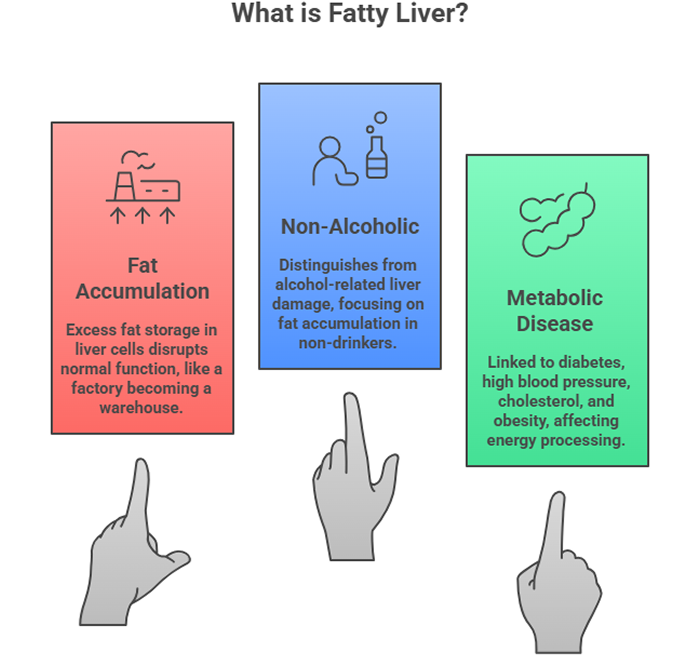
Let me explain this in simple terms. Your liver is supposed to process fats, not store them. But when excess fat starts accumulating inside liver cells, the organ begins to struggle. Think of it like a factory that’s meant to process materials, not warehouse them. When storage takes over, normal operations get disrupted.
The medical term for this condition is Non-Alcoholic Fatty Liver Disease, or NAFLD. The “non-alcoholic” part is important because it distinguishes this condition from liver damage caused by excessive alcohol consumption. We’re talking about a completely different situation here—one where the liver accumulates fat even in people who drink little to no alcohol.
What makes fatty liver particularly concerning is its connection to other health problems. It doesn’t exist in isolation. Most people with fatty liver also deal with diabetes, high blood pressure, elevated cholesterol, or obesity. That’s why doctors now classify it as a metabolic disease—it’s intimately linked with how your body processes energy and stores fat.
The Silent Nature of Fatty Liver
Here’s something that catches most people off guard: fatty liver rarely announces itself with obvious symptoms. In fact, about 80% of people who have it feel absolutely fine. They go about their daily lives with no discomfort, no warning signs, nothing that would make them think something’s wrong with their liver.
This is precisely why so many cases are discovered accidentally. Someone goes for an ultrasound because of kidney stones, or during a routine health checkup, and suddenly there’s this unexpected finding: “You have fatty liver.” The news often comes as a complete surprise.
Now, this doesn’t mean fatty liver never causes symptoms. About 15 to 20% of patients do experience some complaints. The most common is a dull pain or sense of heaviness on the right side of the abdomen, just below the ribcage where the liver sits. Some people describe it as a persistent discomfort that doesn’t quite go away.
When the liver becomes inflamed—which happens in more advanced cases—you might experience nausea or episodes of vomiting. Your appetite might decrease, and you may feel generally unwell without being able to pinpoint exactly what’s wrong.
When Fatty Liver Becomes Serious
I want to be honest with you about something. While most people with fatty liver will never develop serious complications, a small percentage will. In these cases, the condition progresses from simple fat accumulation to something more dangerous.
The progression typically goes like this: First, you have fat in the liver. Then inflammation develops, turning it into what we call non-alcoholic steatohepatitis, or NASH. If this inflammation continues unchecked, it causes scarring—a process called fibrosis. When scarring becomes extensive, it leads to cirrhosis.
Cirrhosis represents severe, irreversible liver damage. At this stage, patients may develop serious complications including fluid accumulation in the abdomen, bleeding from enlarged veins in the esophagus, confusion from toxin buildup, and in rare cases, liver tumors.
But please, don’t let this information terrify you. I’m sharing it not to create panic but to emphasize why early detection and lifestyle changes matter. The vast majority of people with fatty liver who make appropriate changes never reach these advanced stages. Understanding the risks helps motivate change, not paralyze us with fear.
The Connection Between Fatty Liver and Metabolic Health
One of the most important things I want you to understand is that fatty liver doesn’t happen in isolation. It’s part of a bigger picture involving how your body handles energy and stores nutrients.
When you consume more calories than your body needs—especially from sugary foods and refined carbohydrates—your liver converts this excess into fat. Some of this fat gets stored in fat cells, but a significant amount stays in the liver itself. Over time, this accumulation affects liver function.
What’s fascinating is the bidirectional relationship between fatty liver and conditions like diabetes. Fatty liver can contribute to insulin resistance, making it harder to control blood sugar. At the same time, diabetes makes fatty liver worse. They feed into each other, creating a cycle that becomes increasingly difficult to break without intervention.
The same connection exists with high cholesterol and blood pressure. People with fatty liver often have abnormal lipid profiles—high triglycerides and low HDL (the “good” cholesterol). They’re also at increased risk for heart attacks and strokes. This is why addressing fatty liver isn’t just about protecting your liver; it’s about reducing your overall cardiovascular risk.
Getting the Right Tests
If you’ve been told you have fatty liver, or if you’re at risk, proper testing is essential. An ultrasound might detect fatty liver, but it doesn’t tell the whole story. We need to understand how much fat is there, whether inflammation exists, and if any scarring has developed.
Blood tests form the foundation of evaluation. We look at liver enzymes—AST, ALT, and GGT—which become elevated when the liver is inflamed. We also check your complete metabolic panel, lipid profile, and markers of inflammation. These tests give us crucial information about disease activity.
One of the most valuable tools we have now is called a FibroScan. This non-invasive test uses ultrasound technology to measure both the amount of fat in your liver and the degree of fibrosis or scarring. It’s quick, painless, and provides information that previously required a liver biopsy. The FibroScan helps us determine whether lifestyle changes alone will suffice or if medical treatment is necessary.
In some cases, particularly when findings are unclear or when we suspect more advanced disease, a liver biopsy might be recommended. This involves taking a tiny sample of liver tissue for microscopic examination. While it sounds intimidating, it’s a straightforward procedure that provides the most accurate assessment of liver condition.
The Power of Lifestyle Changes
Now we come to the most important part of this entire discussion: what you can actually do about fatty liver. And here’s some genuinely good news—lifestyle modification is remarkably effective.
Weight Loss: The Foundation
If you’re overweight or obese, weight loss is the single most powerful intervention available. Research consistently shows that losing just 5 to 10% of your body weight can significantly reduce liver fat. In many cases, this modest weight loss can completely reverse fatty liver.
Let’s put this in practical terms. If you weigh 90 kilograms, losing 4.5 to 9 kilograms can make a dramatic difference. That’s achievable through consistent effort over several months. You don’t need crash diets or extreme measures. Steady, sustainable weight loss wins the race.
Dietary Changes That Matter
What you eat has a direct impact on your liver. Certain dietary changes make a real difference:
Reduce sugar intake dramatically. This is non-negotiable. Sugary beverages, sweets, and desserts contribute directly to liver fat accumulation. When you cut back on sugar, your liver gets immediate relief.
Eliminate or drastically reduce fried and oily foods. These foods are calorie-dense and promote weight gain. They also contain types of fats that the liver struggles to process efficiently.
Stay away from processed and junk foods. These items typically combine excess calories with poor nutritional value. They also often contain high fructose corn syrup, which is particularly harmful to the liver.
Focus on whole foods. Vegetables, fruits, whole grains, lean proteins, and healthy fats should form the foundation of your diet. These foods provide nutrients your liver needs while supporting weight loss and metabolic health.
Exercise: More Important Than You Think
I need to be completely frank about exercise because this is where many people fall short. Simply taking a casual walk, while better than nothing, isn’t enough to address fatty liver effectively.
What you need is moderate to vigorous exercise that gets your heart rate up and makes you sweat. This means activities like brisk walking where you can still talk but would struggle to sing, jogging, cycling, swimming, dancing, or aerobics classes.
The prescription is specific: 30 to 45 minutes of exercise, at least five days per week. When patients tell me they’re walking for 20 minutes three times a week, I have to gently explain that while that’s a start, it’s not sufficient to reverse fatty liver. We need consistency and intensity.
Why is exercise so crucial? Physical activity helps your body use stored fat for energy. It improves insulin sensitivity, which helps break the cycle of fat accumulation. It reduces inflammation throughout your body, including in your liver. And importantly, it aids weight loss by burning calories.
The Alcohol Question
If you have fatty liver and you drink alcohol, you’re combining two separate threats to your liver. Even moderate alcohol consumption in someone with pre-existing fatty liver can accelerate disease progression significantly.
This is one area where I don’t mince words with patients: alcohol must be completely avoided if you have fatty liver. I understand that social drinking is common and giving it up can be difficult, but your liver’s health depends on it. The good news is that when people stop drinking and make other lifestyle changes, their liver often shows remarkable improvement.
Understanding Stress and Sleep
Two factors that often get overlooked are stress management and sleep quality. Chronic stress elevates cortisol levels, which promotes fat storage, particularly in the abdomen and liver. Finding effective stress reduction techniques—whether through meditation, yoga, counseling, or hobbies—supports your overall health and helps with weight management.
Similarly, poor sleep disrupts metabolic hormones. People who consistently sleep less than six hours per night have higher rates of obesity and metabolic syndrome, both of which worsen fatty liver. Prioritizing 7-8 hours of quality sleep each night is more important than most people realize.
When Medication Becomes Necessary
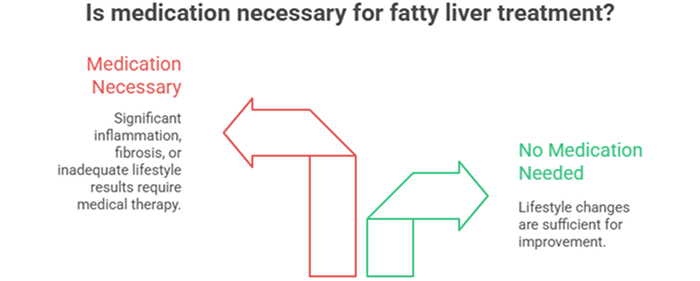
Most people with fatty liver don’t need medication. Lifestyle modification remains the primary and most effective treatment. However, a small percentage of patients require medical therapy, particularly when:
- Significant inflammation is present
- Fibrosis is developing or progressing
- Lifestyle changes alone haven’t produced adequate improvement after several months of genuine effort
Currently, no medication is specifically approved just for fatty liver, though several are under investigation in clinical trials. The medications we do use target associated conditions—diabetes medications that also benefit the liver, vitamin E in certain cases, or medications to address cholesterol problems.
The important thing to understand is that even when medication is prescribed, it works best alongside lifestyle changes. Pills cannot substitute for dietary improvements and exercise. They work together, with lifestyle forming the foundation and medication providing additional support when needed.
The Timeline for Improvement
Patients often ask me how long it takes to see results. The honest answer is that it varies, but most people notice measurable improvements within three to six months of making consistent lifestyle changes.
Blood tests showing liver enzymes often improve within weeks of starting dietary changes. Fat reduction in the liver, measured by FibroScan or ultrasound, typically takes several months to become apparent. Weight loss, when approached sustainably, occurs at a rate of 0.5 to 1 kilogram per week.
The key word here is “consistent.” Starting and stopping, making changes for a few weeks then reverting to old habits—this approach won’t work. Your liver needs sustained, long-term changes to heal and recover.
Moving Forward With Hope
If you’ve been diagnosed with fatty liver, I want you to understand something important: this is largely a reversible condition. Unlike some liver diseases that cause permanent damage, fatty liver responds remarkably well to appropriate interventions.
Yes, it requires effort. Yes, it means changing habits that may have been part of your life for years. But the alternative—allowing the condition to progress—carries real risks that can be avoided.
Start with small, manageable changes rather than trying to overhaul everything at once. Maybe you begin by cutting out sugary drinks and adding a 30-minute walk five days a week. Once those habits are established, you make additional improvements. Progress, even slow progress, is still progress.
Get the proper evaluation and understand where you stand. Work with your healthcare provider to develop a realistic plan. And then commit to following through, not perfectly, but consistently.
Your liver has an remarkable ability to heal itself when given the chance. Give it that chance through the choices you make each day. The power to change your liver’s future is largely in your hands, and that’s actually very good news.
Take Control of Your Liver Health Today
If you’ve been diagnosed with fatty liver or have concerns about your liver health, Dr. Preetha Thomas, a specialist gastroenterologist with expertise in hepatology, provides comprehensive evaluation and personalized treatment plans at her practice in Pretoria. From advanced diagnostic testing including FibroScan to ongoing support for lifestyle modification, you’ll receive expert guidance tailored to your specific needs.
Contact us today to schedule your consultation and take the first step toward better liver health.