Something alarming is happening in medical practices worldwide. As a gastroenterologist, I’ve witnessed a dramatic demographic shift over the past few years. My waiting room, once filled predominantly with middle-aged and older patients, now includes a striking number of people in their 20s and 30s struggling with serious digestive problems.
These young adults arrive with complaints that mirror those of older generations—chronic bloating, persistent abdominal pain, acid reflux, irregular bowel movements, and unexplained digestive distress. The difference? They’re experiencing these conditions decades earlier than their parents or grandparents ever did. What we once considered “middle-age” digestive issues are now appearing in college students, young professionals, and people barely out of their teens.
The statistics tell a sobering story. Nearly 20% of adults under 35 now struggle with irritable bowel syndrome. Inflammatory bowel disease diagnoses in young adults have surged. Emergency room visits for digestive complaints among 18-35 year-olds have increased over 40% in the past decade. We’re witnessing a fundamental shift in when digestive disorders emerge, and understanding why this is happening has become critically important.
The Ultra-Processed Food Takeover
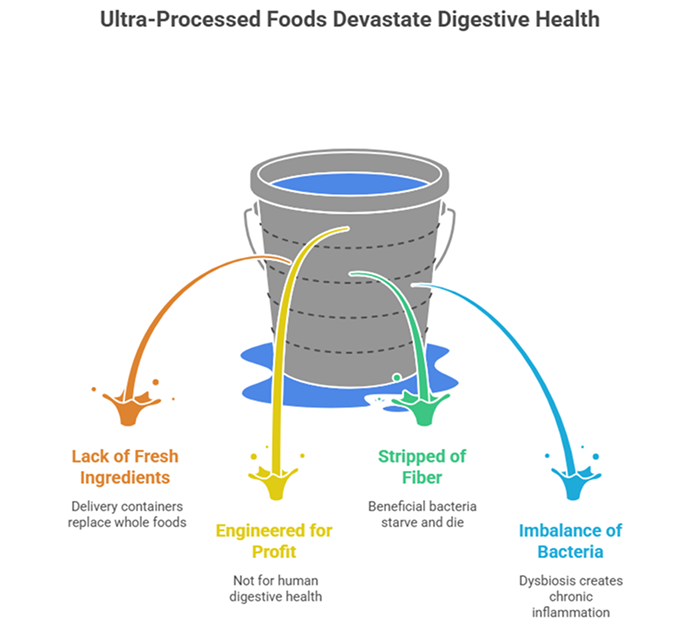
Let’s confront an uncomfortable truth: the way young adults eat in 2026 bears little resemblance to how any previous generation nourished themselves. The rise of ultra-processed convenience foods has fundamentally transformed the modern diet in ways that devastate digestive health.
Open a typical young adult’s refrigerator or pantry, and you’ll find more delivery containers and processed packages than actual ingredients. Breakfast often consists of a grab-and-go processed bar. Lunch arrives via food delivery apps offering the cheapest, fastest options. Dinner might be another delivery order, frozen meal, or restaurant takeout. Home cooking with fresh, whole ingredients has become increasingly rare rather than the daily norm.
These ultra-processed foods are engineered for long shelf life, consistent taste across locations, and maximum profitability—not human digestive health. They’re systematically stripped of fiber, loaded with preservatives and additives, high in inflammatory fats and refined sugars, and designed to be hyperpalatable so consumers eat more than they actually need.
The impact on gut bacteria is devastating. Your beneficial gut bacteria require diverse plant fibers to survive and thrive. When your diet consists primarily of processed foods with minimal fiber variety, these helpful bacteria starve and die off. Meanwhile, bacteria that thrive on simple sugars and refined carbohydrates multiply rapidly. This bacterial imbalance—called dysbiosis—creates chronic inflammation throughout the digestive tract, impairs proper nutrient absorption, weakens the intestinal barrier, and establishes the foundation for long-term digestive disorders.
The Chronic Stress Phenomenon
If one factor truly distinguishes young adults in 2026 from previous generations, it’s the relentless, chronic stress they navigate daily. Economic uncertainty looms with crushing student debt, impossible housing markets, and stagnant wages. Climate anxiety weighs heavily on mental health. Social media creates constant comparison and inadequacy. Political polarization adds layers of tension. The lingering effects of global pandemics continue disrupting normal life patterns.
Young adults today exist in a perpetual state of stress that earlier generations simply never experienced with this intensity or duration. What many people don’t realize is that stress isn’t merely psychological—it produces profound, measurable physical effects on digestive function.
The gut-brain axis means psychological stress translates directly into digestive dysfunction. Chronic stress keeps your body in “fight or flight” mode, continuously diverting blood flow and resources away from digestive processes. This sustained activation fundamentally alters gut bacteria composition, increases intestinal permeability (allowing harmful substances to leak into the bloodstream), changes how quickly food moves through your system, and dramatically heightens pain sensitivity throughout the digestive tract.
The constant stomach noises and gurgling many young people experience often stems directly from stress-induced hyperactivity in their digestive systems. What seems like embarrassing sounds frequently signals deeper dysfunction caused by unrelenting psychological pressure.
The Sleep Deprivation Epidemic
Young adults in 2026 sleep significantly worse than any previous generation. Between demanding work schedules, financial necessity of side hustles, active social lives maintained through screens, digital addiction, and anxiety-driven insomnia, the average person under 35 manages barely six hours of sleep nightly—far below the seven to nine hours human bodies require for optimal function.
This chronic sleep deprivation creates absolute havoc for digestive health in ways most people never connect. Gut bacteria operate on circadian rhythms identical to human sleep-wake cycles. Different bacterial species become active at specific times of day. When sleep is inadequate or occurs at irregular times, these natural biological rhythms become completely disrupted, fundamentally altering bacterial composition and impairing digestive processes.
Sleep deprivation also severely impacts hormones regulating appetite and metabolism. Sleep-deprived bodies produce excess ghrelin (hunger hormone) and insufficient leptin (satiety hormone). This hormonal chaos drives cravings for high-calorie, processed foods that further damage gut health—creating a destructive cycle where poor sleep leads to poor food choices, which cause digestive problems, which worsen sleep quality even more.
During sleep, your digestive system performs critical repair and maintenance work. The intestinal lining regenerates damaged cells. Beneficial bacteria populations expand. Inflammatory processes calm and resolve. When sleep is chronically inadequate, none of this essential repair happens properly, allowing small digestive issues to compound into chronic, potentially lifelong conditions.
The Sedentary Lifestyle Crisis
Previous generations incorporated physical movement naturally into daily life. They walked to destinations, performed physical labor, played outside, and engaged in active recreation. Young adults in 2026 have systematically engineered almost all physical activity out of their existence.
Work happens seated at computer screens for eight, ten, sometimes twelve consecutive hours. Socializing occurs digitally through screens rather than active in-person gatherings. Entertainment streams directly to devices requiring zero movement. Food delivers to doorsteps eliminating even short walks to restaurants. Transportation involves sitting in cars or on public transit. The average young adult now sits motionless for over 10 hours daily, with minimal meaningful physical activity interrupting these sedentary stretches.
This profound lack of movement produces serious digestive consequences. Physical activity stimulates the intestinal contractions moving food and waste through your digestive system. Without adequate movement, transit time slows dramatically. Constipation becomes standard. Food remains in intestines longer, creating perfect conditions for harmful bacterial overgrowth while beneficial bacteria struggle to survive.
The complete absence of regular physical activity in modern young adult life represents a major contributor to the digestive disorder epidemic we’re witnessing. Bodies designed for movement simply cannot maintain healthy digestive function while remaining motionless for most waking hours.
The Hydration Paradox
Despite trendy reusable water bottles being ubiquitous accessories in 2026, genuine chronic dehydration afflicts many young adults. They carry water bottles everywhere but drink from them sporadically at best. Instead, fluid intake comes primarily from coffee, energy drinks, caffeinated beverages, and sugary drinks—none of which provide the hydration digestive systems desperately need.
Adequate water intake is absolutely essential for healthy digestion. Water produces the digestive fluids breaking down food. It maintains the protective mucus lining intestinal walls. It prevents constipation by keeping stool soft enough to pass comfortably. Chronic dehydration makes every digestive process more difficult and less efficient.
The problem extends beyond simply drinking insufficient water. Many young people struggle with poor fluid absorption due to mineral and electrolyte imbalances stemming from nutritionally inadequate diets. They might consume water but still experience dehydration symptoms because their bodies cannot properly absorb and utilize that water without adequate minerals and electrolytes.
The Pressure and Posture Problem
Modern work and lifestyle patterns create physical strain that directly impacts digestive health in ways most people never consider. Hours spent hunched over laptops, slouching on couches while scrolling phones, and maintaining poor posture throughout the day compress abdominal organs and interfere with normal digestive function.
This chronic compression and poor posture can contribute to conditions like hiatus hernia, where increased abdominal pressure causes part of the stomach to push through the diaphragm. The constant physical strain from poor ergonomics, combined with sedentary habits, creates mechanical problems affecting how the digestive system functions.
Additionally, many young adults experience dehydration cramps and digestive discomfort that stems from inadequate hydration and mineral imbalances. Understanding when plain water isn’t sufficient and when you might need electrolyte water becomes crucial for maintaining optimal digestive function, especially during periods of stress, exercise, or in hot climates.
The Screen Time Impact
Young adults average over 11 hours of daily screen time in 2026—a staggering number with profound digestive implications. Screen time affects gut health through multiple interconnected pathways.
First, screens directly displace physical activity. Hours spent scrolling represent hours not spent moving. Second, screen time during meals promotes distracted eating. Watching videos or scrolling social media while eating leads to inadequate chewing, rapid consumption, and complete disconnection from hunger and fullness signals. This eating pattern directly impairs digestion.
Third, evening screen exposure disrupts sleep through blue light and stimulating content consumed before bed. Fourth, the constant information overload, negative news consumption, and social media comparison creates chronic low-level stress manifesting as real physical digestive symptoms.
The psychological toll of constant digital connectivity keeps nervous systems activated in ways that fundamentally impair digestive function. What happens on screens translates directly into what happens in your gut.
The Antibiotic Aftermath
Many young adults received multiple antibiotic courses during childhood and adolescence. While antibiotics save lives when medically necessary, decades of overuse created unintended long-term consequences we’re only now fully recognizing.
Each antibiotic course decimates gut bacteria populations indiscriminately—killing beneficial bacteria alongside harmful ones. While gut microbiomes can recover from occasional antibiotic use, repeated courses throughout developmental years create lasting alterations to bacterial diversity and composition.
Research increasingly demonstrates that early-life antibiotic exposure correlates strongly with higher rates of inflammatory bowel disease, irritable bowel syndrome, and various chronic digestive disorders emerging in young adulthood. These disruptions can also contribute to conditions like hiatus hernia as the weakened digestive system becomes more vulnerable to structural problems. The gut microbiome established during childhood and teenage years influences digestive health throughout the entire lifespan. Disruptions during critical developmental windows produce consequences persisting for decades.
Practical Solutions for Young Adults
Understanding why digestive disorders are surging among young adults matters, but taking action matters more. The encouraging reality is that many contributing factors can be modified through conscious lifestyle changes.
Shift toward whole foods gradually. Perfection isn’t required—small consistent changes create significant impact. Add vegetables to current meals, choose whole grain options, cook at home occasionally. Each small shift helps.
Incorporate daily movement. Expensive gyms aren’t necessary. Walking, home workouts, dancing, recreational sports—any regular activity helps. Aim for 30 minutes daily of movement raising your heart rate.
Prioritize sleep protection. Make quality sleep non-negotiable. Establish consistent bedtime routines, remove screens from bedrooms, create dark, cool sleeping environments.
Develop active stress management. Stress won’t disappear, but coping strategies can improve. Explore therapy, meditation, regular exercise, creative outlets, nature time—find what works and practice consistently.
Maintain proper hydration. Carry water bottles and actually drink from them. Set reminders if needed. Pay attention to hydration quality, not just quantity.
Set screen boundaries. Designate screen-free times and spaces. Both mental and digestive health benefit enormously from these boundaries.
Seek timely medical help. Don’t ignore persistent symptoms hoping they’ll resolve independently. Early intervention prevents small issues from becoming chronic lifelong conditions.
When Professional Evaluation Is Essential
Young adults should consult gastroenterologists for:
- Digestive symptoms persisting beyond a few weeks despite lifestyle modifications
- Blood in stool or vomit
- Unintentional weight loss
- Severe or worsening pain
- Symptoms significantly disrupting daily activities
- Family history of digestive diseases combined with new symptoms
Early diagnosis and appropriate treatment profoundly impact long-term health outcomes. Don’t let embarrassment or assumptions about being “too young for serious problems” delay necessary medical care.
Looking Forward
The surge in young adult digestive disorders isn’t mysterious—it’s the predictable result of how dramatically life has changed within a single generation. Human bodies evolved over millions of years but now face lifestyle patterns that emerged within decades.
This also means solutions exist. By understanding specific factors contributing to digestive dysfunction and making conscious choices countering them, young adults can protect and restore digestive health. Small consistent changes compound into significant long-term improvements.
Your digestive health in your 20s and 30s establishes foundations for your entire life. Choices made now either support lasting wellness or create chronic problems persisting for decades. The power to choose wisely rests in your hands.
Expert Digestive Health Support
If you’re a young adult experiencing persistent digestive problems or want personalized guidance for protecting your gut health, Dr. Preetha Thomas, specialist gastroenterologist in Pretoria, provides comprehensive evaluation and evidence-based treatment plans addressing modern lifestyle challenges.
Contact us today at 012 367 4504/5 to schedule your consultation.