Your great-grandparents probably never worried about their gut health. They didn’t take probiotics, avoid gluten, or struggle with the constant bloating and digestive discomfort that seems to plague modern life. Yet today, digestive issues are practically epidemic. Irritable bowel syndrome, inflammatory bowel disease, acid reflux, and chronic inflammation are all on the rise, affecting people at younger ages than ever before.
What changed? It’s not that our digestive systems suddenly became defective. The problem is that our modern lifestyle—the way we eat, work, sleep, and even relax—is fundamentally incompatible with healthy digestive function. Chronic gut inflammation has become the invisible epidemic of the 21st century, driven by factors our bodies were never designed to handle.
The Perfect Storm: Modern Life Meets Ancient Biology
Your digestive system evolved over millions of years to handle very specific conditions: whole foods gathered from nature, regular physical activity, natural sleep-wake cycles, and manageable, short-term stress (like running from predators, not responding to emails at midnight). Modern life violates nearly every one of these conditions.
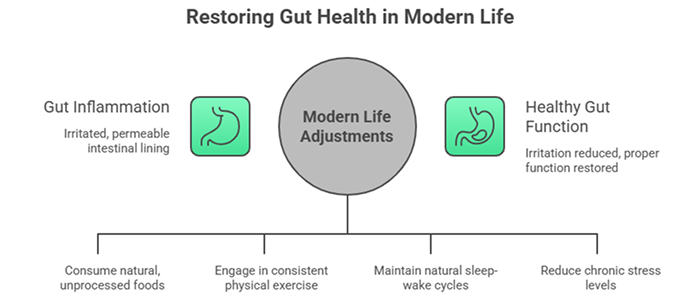
We’re living in bodies designed for the Paleolithic era while navigating a world of processed foods, chronic stress, artificial light, and sedentary behavior. The result is widespread gut inflammation—a state where your intestinal lining becomes irritated, permeable, and unable to function properly. This inflammation doesn’t just cause digestive symptoms. It affects your immune system, mood, energy levels, and overall health in profound ways.
Understanding how specific aspects of modern life contribute to gut inflammation is the first step toward protecting your digestive health in a world that seems designed to undermine it.
The Chronic Stress Epidemic and Your Gut
Let’s start with perhaps the biggest culprit: chronic stress. Your ancestors experienced acute stress—brief, intense threats followed by resolution and rest. Modern humans experience something far more insidious: constant, low-grade stress that never fully resolves.
Work deadlines, financial pressures, relationship conflicts, traffic, news alerts, social media comparisons—the list of chronic stressors is endless. Your body responds to all of these with the same ancient stress response, flooding your system with cortisol and adrenaline. When this happens occasionally, it’s manageable. When it happens constantly, it wreaks havoc on your digestive system.
Chronic stress impacts your gut in multiple devastating ways. It reduces blood flow to your digestive organs, diverting resources to your muscles for “fight or flight.” This compromises your intestinal lining, making it more permeable—a condition often called “leaky gut.” When your intestinal barrier becomes permeable, partially digested food particles, bacteria, and toxins can leak through into your bloodstream, triggering widespread inflammation.
Stress also disrupts your gut microbiome—the trillions of bacteria living in your intestines. These bacteria aren’t just passengers; they’re active participants in digestion, immune function, and even mood regulation. Chronic stress reduces beneficial bacteria while promoting harmful species, creating dysbiosis that perpetuates inflammation.
Perhaps most concerning, stress alters gut motility—how quickly food moves through your system. For some people, this means chronic diarrhea as the stressed gut rushes everything through. For others, it means severe constipation as digestive processes slow to a crawl. Either way, the result is discomfort, inflammation, and impaired nutrient absorption.
The gut-brain connection works both ways, creating a vicious cycle. Gut inflammation sends signals back to your brain, increasing anxiety and stress sensitivity. You become more reactive to stressors, which further damages your gut, which increases your stress response. Breaking this cycle requires addressing both the stress itself and the gut inflammation it causes.
The Modern Diet: Engineered to Inflame
If chronic stress were the only problem, we might stand a chance. But the modern diet compounds the damage exponentially. The foods that dominate Western diets—ultra-processed, sugar-laden, artificially flavored and colored—are fundamentally inflammatory.
Consider what you might eat in a typical day: breakfast cereal with added sugar, a sandwich on refined white bread for lunch, packaged snacks throughout the day, takeout or frozen meals for dinner. Each of these foods contains ingredients your great-grandparents wouldn’t recognize as food: emulsifiers, preservatives, artificial sweeteners, refined oils, and additives designed to increase shelf life and palatability.
These ultra-processed foods disrupt your gut in several critical ways. First, they lack fiber—the indigestible plant material that feeds beneficial gut bacteria. Without adequate fiber, beneficial bacteria starve while harmful species proliferate. This shifts your microbiome toward a pro-inflammatory state.
Second, many additives directly damage the intestinal lining. Emulsifiers (found in ice cream, mayonnaise, and countless processed foods) can degrade the protective mucus layer coating your intestines, increasing permeability and inflammation. Artificial sweeteners, marketed as healthy alternatives to sugar, actually disrupt gut bacteria and impair glucose metabolism.
Third, the high sugar content of modern diets feeds inflammatory bacteria and yeast, promoting their overgrowth. Refined carbohydrates (white bread, pasta, pastries) behave similarly, rapidly converting to sugar in your bloodstream and feeding pathogenic organisms in your gut.
The inflammatory oils used in processed foods—particularly partially hydrogenated oils and excessive omega-6 fatty acids—directly promote inflammation throughout your body, including your gut. Meanwhile, anti-inflammatory omega-3 fatty acids (found in fatty fish, flaxseeds, and walnuts) are often severely lacking in modern diets.
Perhaps most concerning is what’s missing from ultra-processed foods: the diverse array of phytonutrients, antioxidants, and compounds found in whole foods that actively reduce inflammation. When you eat mostly processed foods, you’re not just consuming pro-inflammatory ingredients—you’re missing out on the anti-inflammatory protection that whole foods provide.
Understanding which foods support digestive health versus those that damage it is crucial for managing gut inflammation in modern life.
The Screen Time Factor: How Digital Life Disrupts Digestion
This might surprise you, but your screen habits—how much time you spend on phones, computers, and televisions—directly impact your gut health. The connection isn’t obvious, but it’s profound and multifaceted.
First, screens promote sedentary behavior. When you’re scrolling through social media, binge-watching shows, or working at a computer for hours, you’re sitting still. Your digestive system relies on movement to function properly. Physical activity stimulates peristalsis (the wave-like contractions that move food through your intestines) and promotes healthy gut motility. Prolonged sitting slows everything down, contributing to constipation, bloating, and inflammation.
Second, screen time—particularly before bed—disrupts your circadian rhythms. The blue light emitted by screens suppresses melatonin production, making it harder to fall asleep and reducing sleep quality. But here’s what most people don’t realize: your gut has its own circadian rhythm. The bacteria in your intestines follow predictable daily patterns, with different species being more active at different times.
When you disrupt your sleep-wake cycle with late-night screen use, you also disrupt your gut’s circadian rhythm. This leads to dysbiosis (bacterial imbalance) and increased intestinal permeability. Research shows that even a few nights of poor sleep can significantly alter your gut microbiome composition and increase inflammatory markers.
Third, screens often correlate with mindless eating. How many times have you eaten an entire meal while staring at your phone or TV, barely tasting your food? This matters because digestion actually begins in your brain. When you see, smell, and anticipate food, your brain sends signals that prepare your digestive system—increasing saliva production, releasing digestive enzymes, and optimizing gut motility.
When you eat while distracted by screens, you bypass these preparatory signals. You also tend to eat faster, chew less thoroughly, and consume more than you would if eating mindfully. All of this impairs digestion and promotes inflammation. Poorly chewed food is harder to digest, stays in your gut longer, and provides more opportunity for bacterial fermentation and gas production.
Finally, the content you consume on screens often increases stress. News alerts about disasters, social media comparisons, work emails during supposed downtime—these all activate your stress response, which as we’ve discussed, directly harms your gut.
The Sleep Deprivation Connection
Modern life has dramatically reduced how much we sleep. Artificial lighting, 24/7 entertainment, shift work, and the “hustle culture” that glorifies sleep deprivation have created a chronically sleep-deprived population. This has serious consequences for gut health.
During sleep, your body performs crucial maintenance and repair work, including in your digestive system. Your intestinal lining cells regenerate, your immune system rebalances, and your gut bacteria undergo important metabolic processes. When you consistently sleep fewer than 7-8 hours, these processes are incomplete.
Sleep deprivation increases intestinal permeability, allowing inflammatory compounds to leak through your gut barrier. It alters your gut microbiome composition, reducing beneficial species and promoting pathogenic ones. It also increases cortisol and other stress hormones, compounding the inflammatory effects of daytime stress.
The relationship is bidirectional. Poor gut health disrupts sleep—people with digestive issues often experience worse sleep quality, creating another vicious cycle. Chronic digestive symptoms can make falling asleep and staying asleep difficult, perpetuating both sleep problems and gut inflammation.
Environmental Toxins and the Modern Gut
Beyond diet, stress, and lifestyle, modern environments expose us to countless chemicals our ancestors never encountered. Pesticides on produce, antibiotics in meat, plastic packaging, household cleaners, personal care products—all of these contain compounds that can disrupt gut health.
Antibiotics deserve special mention. While life-saving when necessary, antibiotics are often overprescribed. They don’t discriminate between harmful and beneficial bacteria—they kill both. Even a single course of antibiotics can alter your gut microbiome for months or even years. Repeated antibiotic use, especially in childhood, is strongly associated with increased risk of inflammatory gut conditions later in life.
Food additives like artificial colors, flavors, and preservatives may also contribute to gut inflammation. While individually these additives are considered safe at regulated levels, we have limited understanding of their cumulative effects or how they interact with gut bacteria over time.
Protecting Your Gut in a Modern World
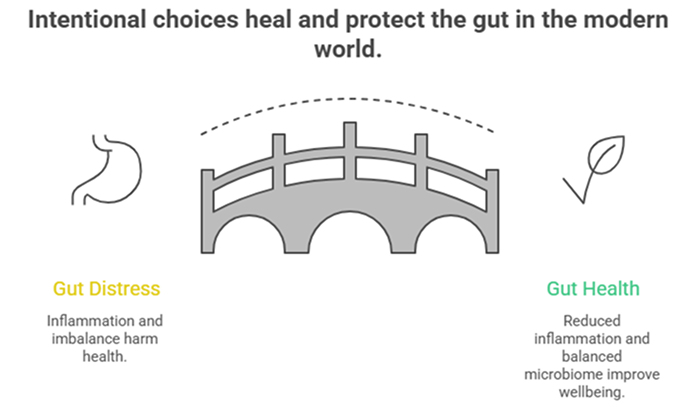
The good news is that you can protect and heal your gut even while living in the modern world. It requires intentional choices, but the impact on your health and wellbeing is profound.
Manage stress actively: Don’t just accept chronic stress as inevitable. Implement regular stress-reduction practices: meditation, deep breathing, yoga, time in nature, therapy, or whatever works for you. Even ten minutes of intentional relaxation daily makes a measurable difference.
Prioritize whole foods: You don’t need a perfect diet, but shifting the balance toward whole, minimally processed foods dramatically reduces gut inflammation. Focus on vegetables, fruits, whole grains, legumes, nuts, seeds, and lean proteins. These provide fiber, nutrients, and anti-inflammatory compounds while avoiding the additives and refined ingredients that damage your gut.
Move regularly: Combat sedentary behavior with regular movement. You don’t need intense workouts—even walking, gentle yoga, or stretching helps stimulate healthy gut motility and reduces inflammation.
Practice digital boundaries: Set limits on screen time, especially before bed. Create phone-free zones and times. Use blue light filters in the evening. Most importantly, practice mindful eating—put devices away during meals and focus on your food.
Protect your sleep: Prioritize 7-9 hours of quality sleep. Maintain consistent sleep-wake times, create a dark, cool sleeping environment, and establish a relaxing bedtime routine without screens.
Support your microbiome: Consider probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi. Eat diverse plant foods to feed beneficial bacteria. If appropriate, high-quality probiotic supplements may help, though whole food sources are ideal.
Be cautious with antibiotics and medications: Use antibiotics only when truly necessary. If you must take them, discuss strategies to protect your gut microbiome with your healthcare provider. Be aware that many common medications can affect gut health.
Stay hydrated: Proper hydration supports the mucus lining of your intestines and helps prevent constipation, both of which protect against inflammation.
When Professional Help Is Needed
While lifestyle changes are powerful, sometimes gut inflammation requires medical evaluation and treatment. Warning signs include persistent abdominal pain, blood in stool, unintentional weight loss, severe or worsening symptoms, or digestive issues that significantly impact your quality of life.
Conditions like inflammatory bowel disease, celiac disease, or severe dysbiosis may require specific medical interventions beyond lifestyle modification. If you’ve implemented healthy changes for several months without improvement, professional evaluation is important.
The Path Forward
Gut inflammation in modern life isn’t inevitable. Yes, we face challenges our ancestors never encountered—chronic stress, ultra-processed foods, sedentary screen-based lifestyles, sleep deprivation, and environmental toxins. But we also have something our ancestors didn’t: understanding of how these factors affect our health and evidence-based strategies to counteract them.
Your gut is remarkably resilient. Given the right conditions—adequate stress management, nourishing whole foods, regular movement, quality sleep, and mindful habits—it can heal and thrive even in our modern world. The key is recognizing that gut health isn’t passive. In an environment that constantly challenges your digestive system, protecting it requires active, intentional choices.
Small changes compound over time. You don’t need to overhaul your entire life overnight. Start with one area—maybe reducing screen time before bed, or adding more vegetables to your meals, or implementing a ten-minute daily meditation practice. As you experience improvements, build on that momentum.
Your digestive health affects everything—your energy, mood, immune function, and overall quality of life. In our modern world, protecting your gut is one of the most important investments you can make in your long-term health and wellbeing.
Get Expert Help for Gut Inflammation
If you’re experiencing persistent digestive symptoms or gut inflammation despite lifestyle changes, Dr. Preetha Thomas, specialist gastroenterologist in Pretoria, provides comprehensive evaluation to identify underlying causes and develop personalized treatment plans that address the root causes of gut inflammation.
Contact us today to schedule your consultation.