Hemorrhoids, a condition often accompanied by discomfort and frustration, affect countless individuals worldwide. Despite its prevalence, the topic remains shrouded in embarrassment and reluctance to seek help. If you’re reading this, chances are you or someone you know is grappling with the challenges posed by hemorrhoids. Fear not, for you’re not alone in this struggle. As a gastrointestinal specialist deeply familiar with the nuances of hemorrhoidal care, I understand the physical and emotional toll it can take.
In this blog, we’ll delve into the world of hemorrhoids, shedding light on what they are, why they occur, and most importantly, how to effectively manage and treat them. Drawing upon my experience in gastroenterology, I’ll share insights into various treatment options that can provide relief and improve quality of life for individuals struggling with hemorrhoids.This guide aims to equip you with the knowledge and tools necessary to address hemorrhoids with confidence and regain control over your health and well-being. So, let’s embark on this journey towards understanding and conquering hemorrhoids, one step at a time.
What Exactly are Hemorrhoids?
Hemorrhoids, commonly referred to as piles, are a prevalent medical condition characterized by swollen veins in the lower rectum and anus. These swollen veins can develop internally, within the rectum, or externally, under the skin around the anus. The root cause of hemorrhoids often lies in increased pressure within the rectal area, leading to the engorgement and swelling of the veins. Several factors can contribute to the development of hemorrhoids by exerting pressure on the rectal area. These factors include:
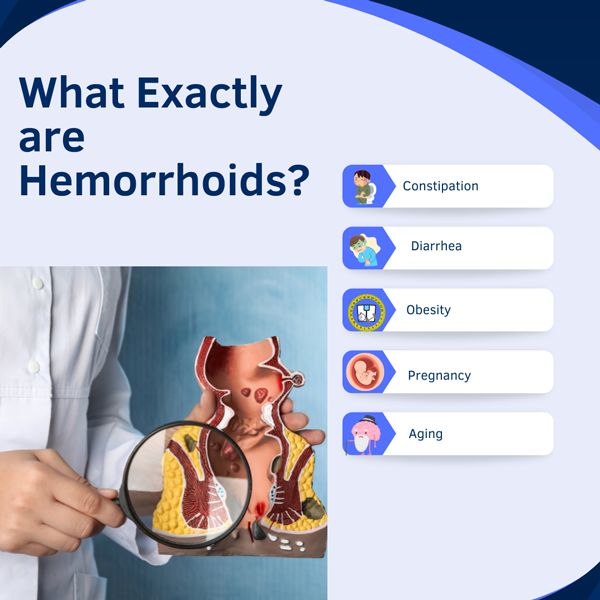
1. Constipation
Chronic constipation, with its irregular or difficult bowel movements, can lead to straining when going to the bathroom. This straining puts extra pressure on the veins near the rectum, which can cause hemorrhoids or make existing ones worse. The increased pressure causes these veins to swell and become inflamed. Therefore, dealing with constipation and is crucial to avoid chronic abdominal pain or discomfort and problems that come with hemorrhoids.
2. Diarrhea
Hemorrhoids can be a consequence of extended bouts of diarrhea. The frequent, loose or inflammatory bowel movements can irritate the sensitive tissues in the rectal area. Even though the strain during bowel movements might be less intense than in constipation, it still puts pressure on the veins around the anus. This ongoing pressure and irritation can make the veins swell and become inflamed, leading to hemorrhoids.
3. Obesity
Being overweight or obese can greatly raise the chance of getting hemorrhoids. The extra weight puts more pressure on the veins in the pelvis and rectum, causing them to become congested and swollen. Moreover, obesity can lead to poor circulation and problems with the veins, making hemorrhoids worse by slowing down blood flow. This combination of increased pressure and poor circulation makes it easier for hemorrhoids to form or get worse.
4. Pregnancy
Pregnancy increases the risk of getting hemorrhoids because of hormonal changes and added pressure on the abdomen. As the uterus grows to accommodate the baby, it presses on the pelvic veins, making blood flow slower and causing congestion in the rectal area. Also, hormonal shifts during pregnancy can weaken vein walls, making them more likely to swell and become inflamed.
5. Aging
As individuals age, the natural weakening of the structures supporting the rectal and anal area can increase susceptibility to hemorrhoids. This weakening occurs as the tissues and muscles in this region lose their flexibility and strength over time. Consequently, the veins become more prone to swelling and inflammation, leading to the development of hemorrhoids. Moreover, ageing and gut health is often accompanied by changes in circulation and bowel function, which can exacerbate the problem. Diminished blood flow and alterations in bowel habits, such as decreased motility or increased constipation, further contribute to the likelihood of experiencing hemorrhoidal issues.
Common Symptoms of Hemorrhoids
- Rectal bleeding, typically during bowel movements
- Itching or irritation in the anal region
- Pain or discomfort, especially during sitting or bowel movements
- Swelling or a lump near the anus
Effective Treatment Options of Hemorrhoids
While hemorrhoids can be bothersome, several treatment options are available to provide relief and promote healing. Here are some effective strategies recommended by gastroenterologists:

1. Dietary Changes
Incorporate a high-fiber diet rich in fruits, vegetables, whole grains, and legumes can significantly improve bowel regularity and stool consistency, reducing the need for straining during bowel movements. Fiber adds bulk to stools, making them softer and easier to pass, which in turn alleviates pressure on the rectal veins and reduces the risk of hemorrhoid formation or exacerbation. Additionally, adequate hydration is essential to maintain stool softness and prevent constipation. Drinking plenty of water throughout the day helps ensure optimal digestion and bowel function. Moreover, avoiding foods that can exacerbate hemorrhoidal symptoms, such as spicy foods, alcohol, and caffeine, can also be beneficial.
2. Topical Treatments
Topical treatments are often used to provide relief from the discomfort and symptoms associated with hemorrhoids. These treatments typically come in the form of creams, ointments, or suppositories that are applied directly to the affected area. Ingredients such as hydrocortisone, witch hazel, lidocaine, or a combination of these can help alleviate itching, inflammation, and pain associated with hemorrhoids. Hydrocortisone, a steroid, works to reduce swelling and inflammation, while witch hazel acts as an astringent, soothing irritation and reducing swelling. Lidocaine, a local anesthetic, helps numb the area, providing temporary relief from pain and discomfort.
3. Medications
Oral pain relievers are often suggested to ease the discomfort of hemorrhoids. When you consult a Gastroenterologist they prescribe medicines that can reduce pain and swelling, making them useful during flare-ups. Stool softeners are also commonly used to make bowel movements less painful by preventing straining. They work by adding more water to stools, making them softer and easier to pass. By reducing the need to strain during bowel movements, stool softeners can help ease symptoms and promote healing of hemorrhoids.
4. Surgical Intervention
In severe cases or when conservative treatments fail to provide relief, surgical removal of hemorrhoids may be necessary. This procedure, known as hemorrhoidectomy, involves the surgical excision or cutting out of the swollen and inflamed hemorrhoidal tissue. Hemorrhoidectomy is typically performed under anesthesia and can be done using various techniques, including traditional surgical excision, laser surgery, or stapled hemorrhoidopexy. While hemorrhoidectomy is considered the most effective treatment for severe hemorrhoids, it is also more invasive and may require a recovery period.
Preventive Measures of Hemorrhoids
Preventive measures are essential for reducing the risk of developing hemorrhoids and preventing recurrent flare-ups. Here are some key preventive strategies individuals can incorporate into their daily routines:
1. Maintain a High-Fiber Diet
Fiber adds bulk to stools, making them softer and easier to pass, which helps prevent constipation and straining during bowel movements. Incorporating plenty of fruits, vegetables, whole grains, and legumes into your meals ensures an adequate intake of fiber. Aim to include fiber-rich foods in each meal and snack throughout the day to support regular bowel movements and reduce the risk of hemorrhoids. Additionally, drinking plenty of water is important when consuming a high-fiber diet to help soften stools and aid in digestion.
2. Exercise Regularly
Regular exercise is essential for maintaining a happy digestive system and can significantly reduce the risk of developing hemorrhoids. Engaging in physical activity promotes healthy digestion and improves circulation throughout the body, including the pelvic region. By increasing blood flow to the rectal area, exercise helps prevent congestion and swelling of the veins, reducing the likelihood of hemorrhoids. Aim for at least 30 minutes of moderate exercise most days of the week, such as brisk walking, swimming, or cycling.
3. Avoid Straining During Bowel Movements
Straining during bowel movements is a significant risk factor for the development of hemorrhoids. This excessive pressure on the rectal veins can lead to swelling and inflammation. To minimize the risk of hemorrhoids, it’s important to take your time on the toilet and avoid pushing or straining excessively. Instead, allow bowel movements to occur naturally and without force. If necessary, using a footstool to elevate your feet while sitting on the toilet can help mimic a squatting position, which may make it easier to pass stools.
4. Practice Good Hygiene
Maintaining proper hygiene of the anal area is crucial for preventing irritation and inflammation that can contribute to hemorrhoids. After bowel movements, it’s important to gently clean the area with mild soap and water or use moistened wipes to remove any fecal residue and bacteria. Avoid using harsh or scented products, as they can irritate sensitive skin and exacerbate symptoms. By keeping the anal area clean and dry, individuals can minimize the risk of developing hemorrhoids and promote overall comfort and well-being.
5. Maintain a Healthy Weight
Being overweight or obese greatly raises the chance of getting hemorrhoids because of the extra pressure on the pelvic and rectal veins. This pressure can cause the veins to become congested and swollen, leading to hemorrhoids. To lower this risk, it’s important to keep a healthy weight through a balanced diet and regular exercise. Eating lots of fruits, vegetables, whole grains, and lean proteins, while cutting down on processed foods and sugary drinks, can help maintain a healthy weight.
6. Avoid Prolonged Sitting or Standing
Sitting or standing for too long can harm blood flow in the pelvic area, increasing pressure on the rectal veins and the risk of hemorrhoids, especially for those with desk jobs. To ease pressure and boost circulation, take breaks to move and stretch regularly. Short walks, stretching, or even standing up and stretching your legs can help. Using a standing desk or ergonomic chair can also help alternate between sitting and standing.
Final Words
Struggling with hemorrhoids can be a daunting experience, but it’s important to remember that relief is attainable with the right approach. Gastroenterologist, have witnessed the impact of hemorrhoids on individuals’ lives and understand the importance of seeking professional advice. By consulting with experts like Dr. Thomas and exploring the range of effective treatment options available, you can take proactive steps towards alleviating discomfort and reclaiming your well-being. Remember, you don’t have to navigate this journey alone. With guidance and support, you can overcome the challenges posed by hemorrhoids and emerge stronger and more comfortable than ever before.