Let’s talk about something most people don’t want to discuss but absolutely should—your bowel movements. I know, I know. It’s awkward. It’s uncomfortable. It’s the last thing you want to read about over breakfast. But here’s the truth: bowel health is a critical indicator of your overall wellbeing, and millions of people suffer in silence with problems that could be addressed.
In my years as a gastroenterologist, I’ve heard countless stories of people whose quality of life is seriously diminished by bowel issues. They plan their entire day around bathroom access. They decline social invitations. They live with constant discomfort. And often, they suffer for months or even years before finally seeking help because they’re too embarrassed to talk about it.
So let’s break through that embarrassment right now. Your bowel movements are a normal bodily function, just like breathing or sleeping. When things aren’t working properly, it affects everything—your energy, your mood, your productivity, and your ability to enjoy life. Understanding common bowel issues and knowing what to do about them isn’t just medical knowledge—it’s self-care.
What “Normal” Actually Means
Before we dive into problems, let’s establish what normal bowel function looks like. And here’s the first important point: “normal” has a surprisingly wide range.
Some people have bowel movements three times daily. Others go once every three days. Both can be perfectly normal, as long as it’s consistent for you and the stools are well-formed and easy to pass. The “you should go once daily” rule that many people learned isn’t actually medically accurate.
What matters more than frequency is:
- Consistency—your pattern stays relatively stable
- Ease—you don’t have to strain excessively
- Completeness—you feel empty afterward, not like there’s more to come
- Comfort—the process isn’t painful
The Bristol Stool Chart, which classifies stool into seven types, is actually a useful medical tool. Types 3 and 4—sausage-shaped and smooth, or snake-like and smooth—represent ideal stool. If your stools consistently fall into these categories and you’re comfortable, you’re doing well.
But when things deviate from your normal pattern, or when you’re experiencing discomfort, that’s when bowel issues start affecting daily life.
Constipation: More Than Just Infrequent Bowels
Constipation is probably the most common bowel complaint I hear. But it’s also the most misunderstood. Many people think constipation simply means not going every day. In reality, medical constipation is defined by several possible symptoms:
- Fewer than three bowel movements per week
- Hard, dry stools that are difficult to pass
- Straining for more than 25% of bowel movements
- Sensation of incomplete evacuation
- Feeling blocked or needing manual assistance
You can technically go daily and still be constipated if you’re straining intensely or passing small, hard pellets. Conversely, going every three days with easy, complete bowel movements isn’t necessarily a problem.
Why it happens:
Modern life is perfectly designed to cause constipation. We sit all day. We ignore the urge to go because we’re busy. We don’t drink enough water. We eat processed foods low in fiber. We’re constantly stressed. All of these factors slow down intestinal movement.
Many people also develop what I call “bathroom anxiety”—they’re so uncomfortable using public restrooms that they habitually suppress the urge. Over time, this trains your body to ignore signals, making constipation worse.
Medications contribute too. Pain relievers, antidepressants, blood pressure medications, iron supplements—the list of constipation-causing drugs is surprisingly long. If your constipation started after beginning a new medication, that’s probably not a coincidence.
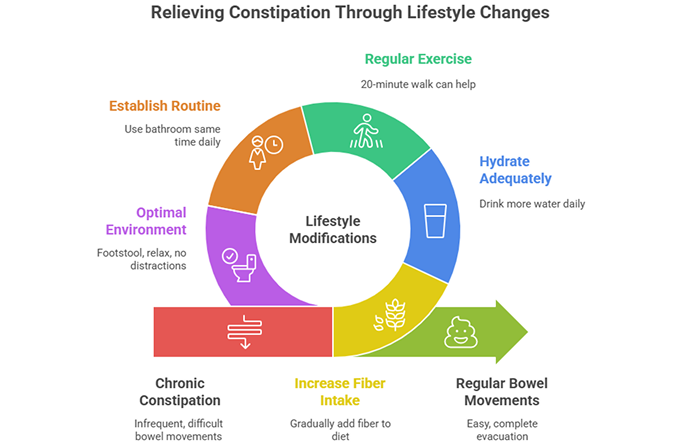
What helps:
Start with the basics: increase fiber gradually (sudden increases cause bloating), drink more water, and move your body. Even a 20-minute walk daily can make a significant difference. Establish a routine—try to use the bathroom at the same time daily, ideally after breakfast when your colon is naturally most active.
Create an optimal bathroom environment. Use a footstool to elevate your feet, which changes the angle of your rectum and makes passing stool easier. Don’t rush. Don’t scroll through your phone. Just relax and let your body do what it needs to do.
If these changes don’t help within a few weeks, it’s time to see a doctor. Chronic constipation can have underlying causes that need proper evaluation.
Diarrhea: When Everything Moves Too Fast
On the opposite end of the spectrum, we have diarrhea—loose, watery stools that come urgently and frequently. While occasional diarrhea from food poisoning or a stomach bug is normal, chronic or recurrent diarrhea significantly impacts daily life.
People with chronic diarrhea often describe their world shrinking. They become hyperaware of bathroom locations everywhere they go. They avoid certain foods, situations, and activities. The constant urgency creates anxiety, which ironically can make the diarrhea worse.
Common causes:
Food intolerances top the list. Lactose intolerance affects a huge percentage of adults. The body stops producing enough lactase enzyme to digest milk sugar, and undigested lactose ferments in your intestines, causing gas, bloating, and diarrhea. Many people don’t realize dairy is their problem because symptoms can be delayed.
Artificial sweeteners, particularly sorbitol and mannitol, are notorious diarrhea triggers. Check your sugar-free gum, diet sodas, and “light” products—these sweeteners draw water into your intestines, causing loose stools.
Stress and anxiety directly affect bowel function. The gut-brain connection means that psychological stress manifests as physical digestive symptoms. Many people experience “nervous diarrhea” before important events or during stressful periods.
Conditions like irritable bowel syndrome (IBS), inflammatory bowel disease, celiac disease, or bacterial overgrowth can all cause chronic diarrhea. If your symptoms persist despite dietary changes, medical evaluation is necessary.
What helps:
Keep a food diary to identify triggers. Common culprits beyond dairy include caffeine, spicy foods, fatty foods, and high-FODMAP foods like onions, garlic, and certain fruits. Understanding food sensitivities helps pinpoint your specific triggers.
Stay hydrated—diarrhea depletes fluids and electrolytes rapidly. Plain water isn’t always enough; you need to replace salts too. Oral rehydration solutions or even diluted sports drinks can help.
Avoid making it worse with common mistakes: don’t eat large meals (smaller, frequent meals are better), don’t consume high-fiber foods during acute episodes (they can increase diarrhea), and be careful with anti-diarrheal medications unless a doctor recommends them.
Irregular Bowel Movements: The Unpredictable Pattern
Some people don’t have consistent constipation or diarrhea—they alternate between both, or their bowel habits are simply unpredictable. One day everything seems fine, the next day brings cramping and urgency. This irregularity can be even more disruptive than a consistent problem because you never know what to expect.
This pattern often points to IBS, a functional disorder where the intestines are structurally normal but don’t function properly. The bowel becomes hypersensitive, responding to triggers that wouldn’t bother most people.
Common triggers:
Stress is huge. Many people with IBS can track their symptoms directly to stressful life events or periods. The gut-brain connection is particularly strong in IBS patients.
Certain foods trigger flares, though which foods vary by individual. The low-FODMAP diet has helped many people identify their specific triggers, though it’s quite restrictive and should be done under professional guidance.
Hormonal changes affect many women. Symptoms often worsen during menstruation when hormone fluctuations alter gut motility.
Sleep disruption, travel, schedule changes—anything that throws off your routine can trigger irregular bowel patterns. Your digestive system thrives on consistency.
What helps:
Establish routines wherever possible. Eat meals at consistent times. Maintain regular sleep schedules. Create morning rituals that give your body time to wake up and empty naturally.
Identify and avoid your personal triggers, but don’t become so restrictive that your diet becomes nutritionally inadequate or your life becomes small. Balance is key.
Consider probiotics. While research on probiotics for IBS shows mixed results, many people find certain strains helpful. It often requires trial and error to find what works for you.
Learn stress management techniques that work for you—whether that’s meditation, exercise, therapy, or creative outlets. Managing stress isn’t just good for your mental health; it’s essential for your bowel health.
Bloating and Gas: The Uncomfortable Companions
While not technically bowel movement issues, bloating and gas often accompany bowel problems and significantly affect daily comfort. That tight, distended feeling makes clothes uncomfortable and kills your confidence.
Gas is normal—everyone produces it. But excessive gas or painful bloating suggests something’s off balance.
Common causes:
Swallowing air while eating, especially if you eat quickly or talk while chewing, introduces gas from above. Certain foods—beans, cruciferous vegetables, carbonated drinks—naturally produce more gas during digestion.
Gut bacteria fermenting undigested food produces gas. If your gut microbiome is imbalanced or if you’re not digesting certain foods properly, fermentation increases.
Constipation causes gas to get trapped behind stool, leading to painful bloating. Once bowel movements normalize, bloating often improves dramatically.
What helps:
Eat slowly and chew thoroughly. This simple change reduces air swallowing and improves initial food breakdown, reducing fermentation.
Identify gas-producing foods in your diet. You don’t necessarily need to eliminate them entirely—often just reducing portions or changing preparation methods helps. Soaking beans overnight, for instance, significantly reduces their gas-producing compounds.
Address underlying constipation or irregular bowel patterns. Gas and bloating are often symptoms of these larger issues.
The Embarrassment Factor: Breaking the Silence
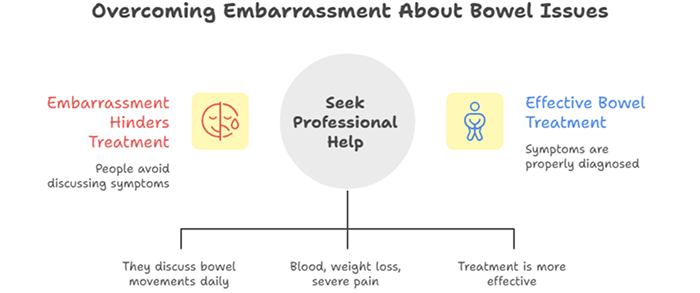
One of the biggest obstacles to addressing bowel issues is embarrassment. People endure years of discomfort rather than discuss their symptoms with a doctor. They try every over-the-counter remedy and internet solution before finally seeking professional help.
I want you to understand something: gastroenterologists talk about bowel movements all day, every day. It’s literally our job. We’ve heard everything. Nothing you could tell us is shocking or unusual. What seems mortifyingly embarrassing to you is completely routine to us.
Moreover, bowel symptoms can indicate serious conditions that need proper diagnosis. While most bowel issues aren’t dangerous, some are. Certain symptoms require prompt evaluation:
- Blood in your stool (red or black)
- Unintentional weight loss
- Severe abdominal pain
- Bowel habit changes that persist more than a few weeks
- Symptoms that wake you from sleep
- Family history of colon cancer with new symptoms
These warning signs shouldn’t be ignored due to embarrassment. Early detection makes treatment more effective.
Lifestyle Factors That Matter More Than You Think
Beyond specific conditions and treatments, several lifestyle factors profoundly affect bowel health:
Diet quality: Processed foods, while convenient, lack the fiber and nutrients your digestive system needs. Whole foods—vegetables, fruits, whole grains, legumes—provide fiber that feeds beneficial gut bacteria and promotes healthy bowel movements.
Hydration: Your colon absorbs water from waste. If you’re dehydrated, it absorbs too much, causing hard, difficult-to-pass stools. Adequate hydration is essential for bowel health.
Physical activity: Exercise stimulates intestinal contractions, moving waste through your system more efficiently. Sedentary lifestyles contribute to constipation and sluggish digestion.
Sleep quality: Poor sleep disrupts the gut microbiome and affects digestive hormone production. Your bowels function best when you’re well-rested.
Stress management: Chronic stress directly impacts gut motility, sensitivity, and microbiome composition. It’s not just “in your head”—stress manifests as real, physical digestive symptoms.
When to Seek Professional Help
Don’t wait until symptoms become unbearable. Seek medical evaluation if:
- Symptoms persist despite lifestyle modifications
- Bowel habits change suddenly and dramatically
- You experience any warning signs mentioned earlier
- Symptoms significantly impact your quality of life
- You’re constantly worried about your bowels
A gastroenterologist can perform appropriate tests to rule out serious conditions and develop a treatment plan tailored to your specific situation. Often, simple interventions make a huge difference once the underlying cause is properly identified.
Taking Control of Your Bowel Health
Your bowel health affects your daily life in countless ways. When things aren’t working properly, it impacts your energy, mood, productivity, and ability to enjoy activities. But bowel issues don’t have to be a permanent sentence of discomfort.
Most bowel problems improve significantly with attention to diet, hydration, exercise, and stress management. Understanding what’s normal for you, recognizing when things are off, and knowing when to seek help empowers you to maintain good bowel health.
Don’t suffer in silence due to embarrassment. Your bowel movements are an important health indicator. Taking care of your digestive system is taking care of yourself. You deserve to feel comfortable in your body and confident in your daily life.
Your bowels are talking to you every day. It’s time to listen.
Expert Bowel Health Evaluation
If you’re experiencing persistent bowel issues affecting your daily life, Dr. Preetha Thomas, specialist gastroenterologist in Pretoria, provides comprehensive evaluation and personalized treatment plans to help you achieve comfortable, healthy bowel function.
Contact us today to schedule your consultation.